A Day in the Life of a Nurse Anesthesia Student
Dené Dainotto, a third-year student in UB School of Nursing's DNP program, provides an account of a day in her life as she navigates her final year of the nurse anesthesia program.
On this page:
CRNAs (Briefly) Defined
Before we talk about a day in my life, I want to describe what a certified registered nurse anesthetist (CRNA) is. CRNAs are advanced practice nurses who provide over 45 million anesthetics each year in the United States and are responsible for safely administering anesthesia to patients before and during procedures and surgeries and for monitoring recovery. A CRNA must work as a baccalaureate-prepared registered nurse (RN) in critical care for a minimum of one year (full time) before (s)he can be accepted into graduate school. The length of this experience requirement varies by program – I personally worked for over five years as an RN before I applied to the program, four of which were in the Intensive Care Unit.
After a rigorous graduate program and meeting or exceeding the required 2,000 clinical hours – which, again, varies by program – nurse anesthesia program graduates become board certified experts who care for and provide every type of anesthesia to patients of all ages and illnesses.
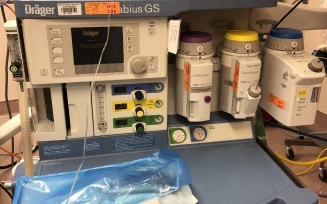
Pictured below is some of the equipment CRNAs use for pediatric patients (left) and adult patients (right).


CRNAs are trained to maintain vigilance while providing anesthesia so they can recognize and immediately respond to any change in patient condition. CRNAs collaborate with surgeons, dentists, physicians and all other members of the health care team to make an individualized anesthesia plan for each patient. They then spend the entire surgery at the head of the bed watching every heartbeat, every breath and various other vital signs to ensure their patient is hemodynamically stable, comfortable and safely anesthetized. Sometimes it’s necessary to wear uncomfortable and awkward equipment to ensure our safety as well. This includes things like lead aprons to protect ourselves from radiation and helmets to protect ourselves from UV lights.


Nurse anesthetists wear scrubs and protective coverings to maintain a sterile surgical environment and to prevent coming in contact with fluids.
CRNAs carry a lot of responsibility and must develop a plethora of skills and knowledge throughout their education programs and careers – while this is a demanding profession, it is also extremely rewarding!
DNP Nurse Anesthetist Program: The Path to the Final Year
I’m currently beginning my third and final year of graduate school at the University at Buffalo (UB) School of Nursing where I will graduate with my Doctorate of Nursing Practice (DNP) in nurse anesthesia. At UB, we take classes throughout the entire year for all three years with a week or two break between each semester.
Once we begin clinical rotations in our second year, we are expected to make it to our site every day that we are scheduled. Even when the city is seemingly shut down for one of Buffalo’s blizzards, with the university closed and travel bans everywhere, we must make a true, honest effort to go into clinical because, as we all know, hospitals don’t close. Attending a nurse anesthesia program is a major commitment and having a good support system is vital to succeeding.
The first year of UB’s program is spent with didactic work consisting of anesthesia courses, advanced nursing practice courses, and an abundance of leadership, research, and writing courses required as DNP coursework. During our second year, we continue to take classes each semester, both anesthesia classes and DNP required courses, and we begin clinical four days a week to learn the art and skill of anesthesia. We work in the operating room alongside a CRNA, an anesthesiologist or both in a team model, where an anesthesiologist is available if needed and watches over multiple cases at once.
In my first clinical year alone, I clocked over 1,400 hours. Those of us attending UB have the advantage of greatly exceeding the 2,000 clinical hour requirement to sit for the board examination. Our third year is spent continuing clinical four days a week, with one semester being three days a week, as we begin our DNP Project research and study. We also continue anesthesia courses and DNP courses in our last year while studying for our boards.
The Insight of Many Sites
The beginning of each semester means a new clinical site. We rotate through two to three clinical sites per semester, which means we change sites every four to nine weeks. I’m on my seventh site and continue to learn more each day. Each site is full of new faces, new equipment and sometimes new anesthesia machines we must learn how to operate. These are just four of the six (or more?) anesthesia machines I’ve learned how to use so far. They might all look the same to someone who isn’t used to looking at them, but each one is different and it takes time to adapt.
A Day in the Life
Beginning the Day Before, at the End
The beginning of each day starts the evening before when we research our patients so we can provide safe anesthesia care specific to each patient. We look up everything we can, including test results, medications and supplements the patient is on, comorbidities, surgical history, allergies, and the surgery at hand. We then make a plan of care for each patient. This includes the aforementioned information in addition to the medications we plan to give, the type of anesthetic and type of airway we’re planning, expected hydration status and fluids needed, lines we may need, expected blood loss, and the position during surgery. This takes 30 to 60 minutes per case.
Because our day starts the day before, my “day in a life” will begin at 3:30 p.m. I finish up my cases for the day, which today consisted of multiple plastic surgeries, and I head to somewhere quiet so I can decompress and focus more on the task at hand. I access my assignment and patients’ charts in the break room; tomorrow I will be in the vascular room. Vascular patients are typically sick patients with a lot of comorbidities to consider. I write a preoperative note and begin the preoperative anesthesia assessment on each patient scheduled in my room tomorrow by going through the charts. This takes me to about 4:15 pm.
It’s important to lead as healthy of a lifestyle as possible while in a nurse anesthesia program so your mind and body are prepared to handle the marathon. Therefore, after I look up my patients’ information, I head to the gym. Workouts are a great way to nurture yourself and let go of some of the stress from the day!

UB’s program has some distance clinical sites where we have a temporary home away from home Tuesday through Friday. I’m currently away from home, so I get back to my hotel around 5:30 p.m. We all try to make the best of our situation no matter where we are and we always have each other to lean on even when we’re far from home.
I didn’t get an opportunity to eat lunch today so I’m ravenous and I scarf down my “lunch.” I get to my room and log my today’s cases. Each day we must log how many hours we were in clinical and specifics about each case, such as the type of surgery, the medications we gave, the type of airway we used, the lines, any nerve blocks, and the monitoring techniques used.
I then take a shower. This brings me to 7:00 p.m. I begin to look up different techniques for the vascular cases I will be in tomorrow so I’m fully prepared.
By 8:00 p.m. I’m done with my clinical work and I begin to do some Apex Anesthesia modules.
This is a board review program geared toward CRNA boards. In addition to all of the other coursework and clinical work, each semester we are also required to complete different modules to help us review old material and also learn new material. As you can imagine, there’s a lot of studying involved in a nurse anesthesia program. In fact, I’ve done so much reading my first two years that my eyeglass prescription (which has been the same since I was in fifth grade) has changed twice since I began my program!
I wind down and am in bed by 10:00 p.m.
The Next Morning: Meetings and Sinatra
My alarm goes off at 5:00 a.m. I try to look alive; I grab my lunch and anything I need for clinical and I’m out the door. I park my car at 5:45 a.m. and am changed and in the OR to set up for the day around 6:00 a.m. If we’re lucky, we arrive before anyone else and we have some quiet time to set up and listen to our music of choice (Frank Sinatra anyone?).
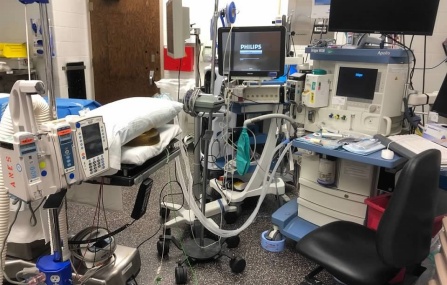
The OR at the beginning of my day.
Today we thought we had a meeting before our cases so I wanted to make sure everything was ready before the meeting. To our surprise, the meeting was cancelled. I have two scheduled AV fistula creations, which is the connection of an artery and a vein to use for dialysis, followed by an EGD, which is when GI doctors will put a camera into the mouth to look all the way down to the beginning of the intestines. These are all planned sedation cases, but it’s important to set up everything for a general anesthetic in case of an emergency.
Machine Check
Each morning I run a machine check on my anesthesia machine to make sure it’s working correctly. The gases we use come from pipelines, but we also check the oxygen, air and nitrous tanks to ensure they’re filled in case of an emergency. I make sure there is an AMBU (artificial manual breathing unit) bag in my room in case of machine or electrical failure.
To set up my rooms I use the mnemonic “SCOMLADIE” that Professor Korogoda taught me.
- Suction: Ensure the suction is nearby and on in case it’s needed quickly to suction secretions or vomit.
- Circuit: Make sure the soda lime isn’t exhausted because this is what prevents rebreathing of CO2. Make sure the scavenger is on to remove any anesthetic gases from the room, and the circuit and filter are new.
- Oxygen: Check the tanks and pipeline pressures.
- Mask and monitors: Make sure I have a pulse oximeter, a blood pressure cuff, EKG leads, a nerve stimulator, an IV pump, a warming blanket, a temperature monitor, and any special monitors.
- Laryngoscope and blades: Check to make sure they’re functioning in case I need to insert a breathing tube.
- Airway: Prepare a breathing tube, oral or nasal airways, and any other airway device that may be needed.
- Drugs: Fill up my anesthetic gases and draw up all of my IV induction medications.
- IV access and fluids: Ensure I have extra fluids in the room, a fluid warmer and supplies for another IV.
- Eyes and positioning: Check for the supplies I’ll need to protect the patients face and eyes during the procedure and check for anything that may be needed for positioning to make sure the patient is safe and nerve injuries won’t occur.
As you can see, there’s a lot to do each morning and a lot of preparation before cases! We can’t just show up and do anesthesia in our small work area in the OR. Once I’m done setting up, I have some extra time so I grab the most important meal of the morning: coffee.
On the Case(s)
The first AV fistula went smoothly. The patient had a nerve block to block the nerves of the arm and decrease the need for other medications and opioids during surgery. The block worked perfectly and a touch of IV midazolam, fentanyl and propofol kept the patient comfortable and without anxiety throughout the case.
The second case was canceled because the patient missed dialysis treatment yesterday. This means we’re not quite sure what else we’ll get today! I’m constantly reminded of the importance of going with the flow and being flexible.
Next, we did our EGD (aka esophagogastroduodenoscopy), which also went smoothly. We did IV sedation with a different combination of drugs because we tailor each anesthetic to each patient. This time we selected midazolam, fentanyl and Precedex. This case also went well.
We then had an add-on case to remove hardware surgically placed in the jaw. We pondered multiple different plans for anesthesia and decided a general anesthetic was the safest for this patient. We planned for a difficult airway. In the room we had a selection of orotracheal tubes, nasotracheal tubes, a glidescope and a fiberoptic bronchoscope all ready to go. After discussion with the surgeon we agreed on an orotracheal tube. We brought the patient back to the OR and hooked up all our monitors. We ensured the surgeon was at the bedside for induction of anesthesia and intubation; this is a safety measure in case a surgical airway is needed. Next up: induction and intubation.

Induction went smoothly and intubation was easier than expected! Just like anything else, when you have everything ready in case of an emergency you ward off bad luck! Once the patient was settled and the case was started, it was 1:00 p.m. and the CRNA I was working with sent me on a lunch break.
My lunch break was spent eating while looking up my cases for tomorrow. I’ll be doing oral and maxillofacial surgeries. It looks like a much healthier group of patients, but concerns still arise as I consider things that could go wrong. I head back to the OR to finish my case. The rest of this case ended smoothly and the patient was stable. Once the patient breathed off the anesthetic gases, had their muscle relaxation reversed, was able to breathe adequate breaths on their own, and was able to follow commands, we removed the breathing tube and brought the patient to recovery.
Ending, and Beginning Again
I was sent home at 3:00 p.m. when my room was finished. I went to the gym and then to my hotel to study outside while the sun was still out. I continued my daily routine and looking up anything I was concerned about and anesthesia options for the cases I’m scheduled to tomorrow so I can begin all over again in the morning.
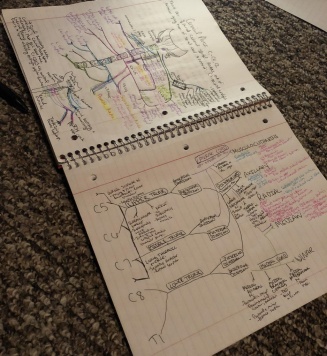
My drawing is on the left, and my significant other's artwork is on the right.
The last two years have flown by with how busy we’ve been, and I’m optimistic this last year will fly as well. Through all the craziness I know I made the right decision beginning a nurse anesthesia program. I’m lucky to have a support system of people who understand when it sometimes takes me weeks to respond to their texts or calls. If you’re ever ignored by a nurse anesthetist student, don’t take offense! Most of the time we’re just barely getting by.
I am beyond appreciative of my supportive and understanding family and friends and my significant other who is beginning nursing school this fall to become an RN. It’s fun to be able to teach and learn from someone also joining the medical field. Sometimes we’re lucky to learn different depths of the same material at the same time, and these are the times I’m reminded that he is a much better artist than me.
-Dené Dainotto, BS, RN (UB SON DNP Nurse Anesthetist Program)